Clinical features
•Essentially, a clinical diagnosis
•Presents as an erythematous scaly or crusted plaque clinically mimicking psoriasis & presenting on the head, neck & extremities; often affecting sun-exposed surfaces
•Anogenital Bowen’s disease is discussed in a seperate blog
•Single or multiple lesions, often many cm in diameter
•Middle-aged or elderly
•No significant sex predilection
•Pigmented variant
•Immunosuppression related cases
•5% develop invasive tumor with significant metastatic potential (30%)

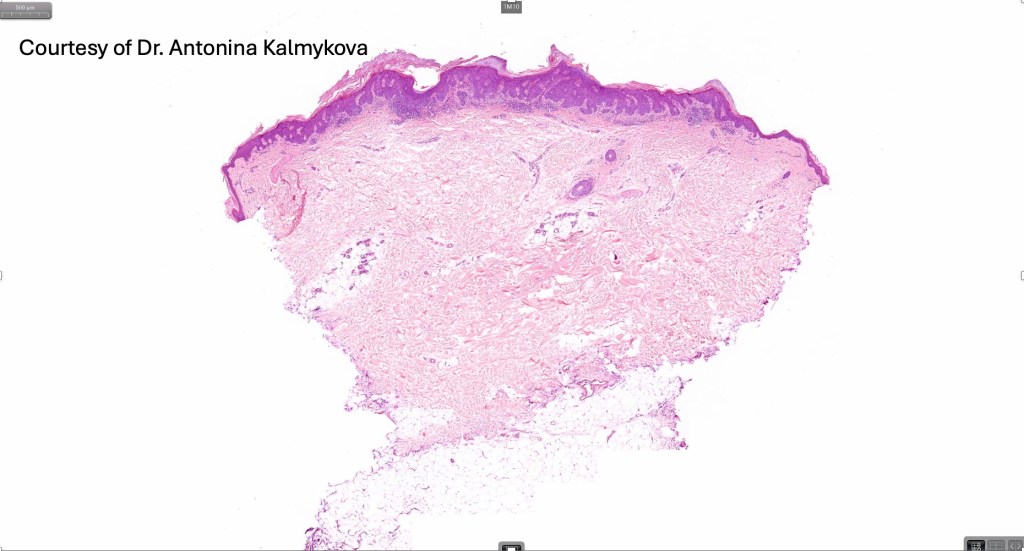
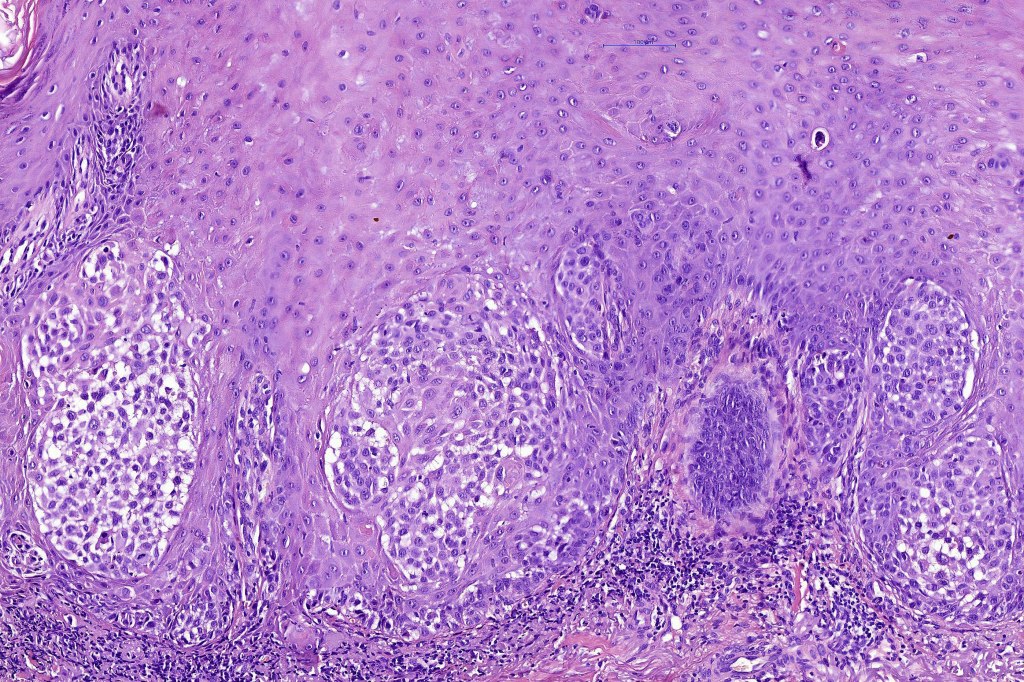
Histological features
•Etiology includes UVB, ionizing radiation, arsenic, HPV infection & immunosuppression
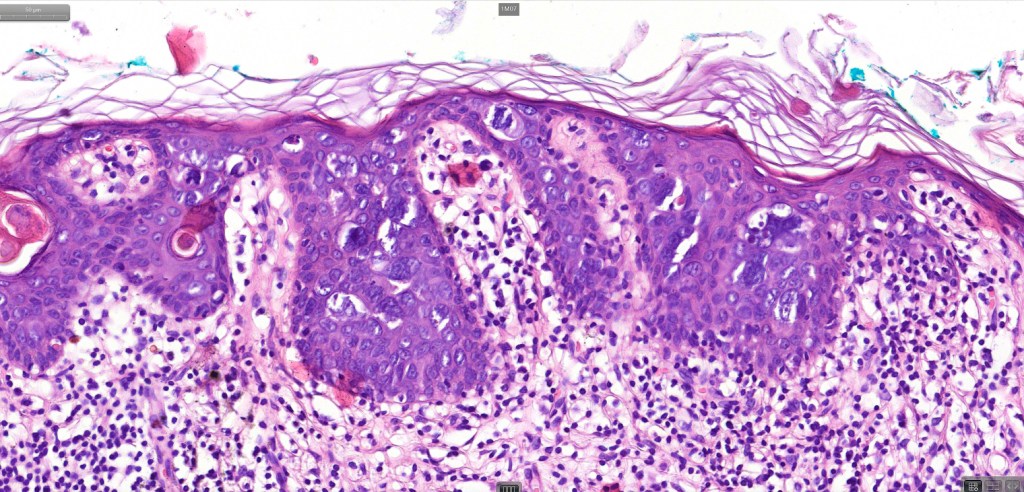
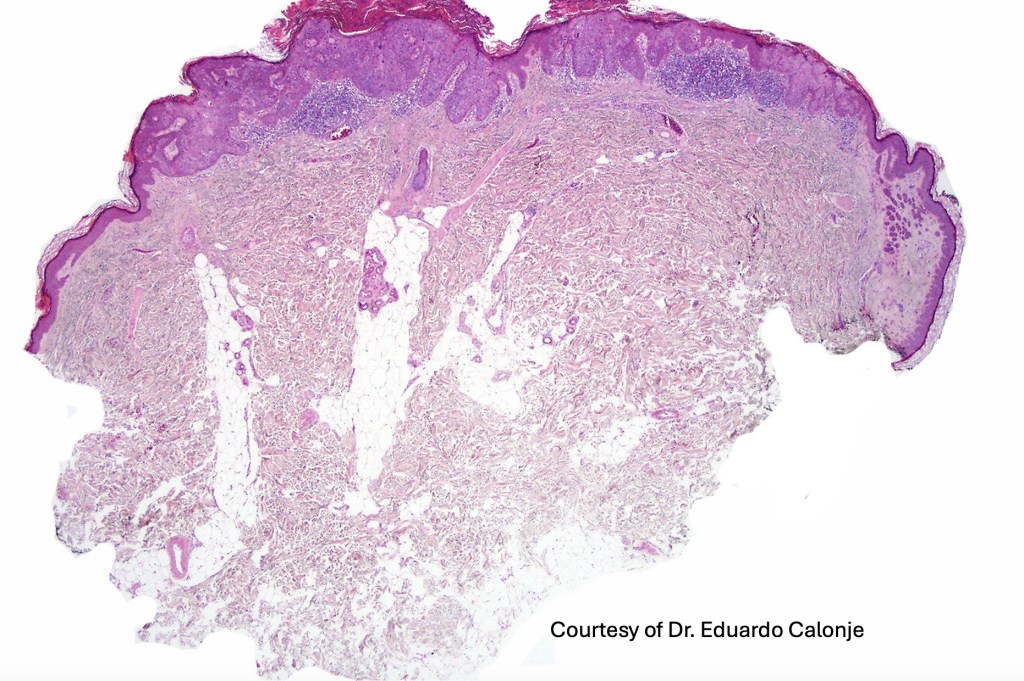
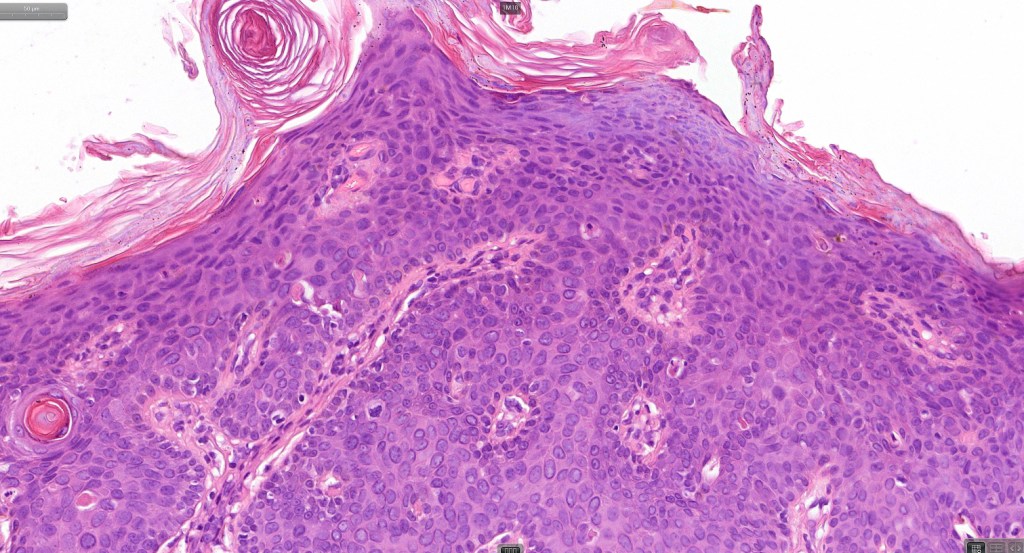
•Hyperkeratosis, parakeratosis & acanthosis
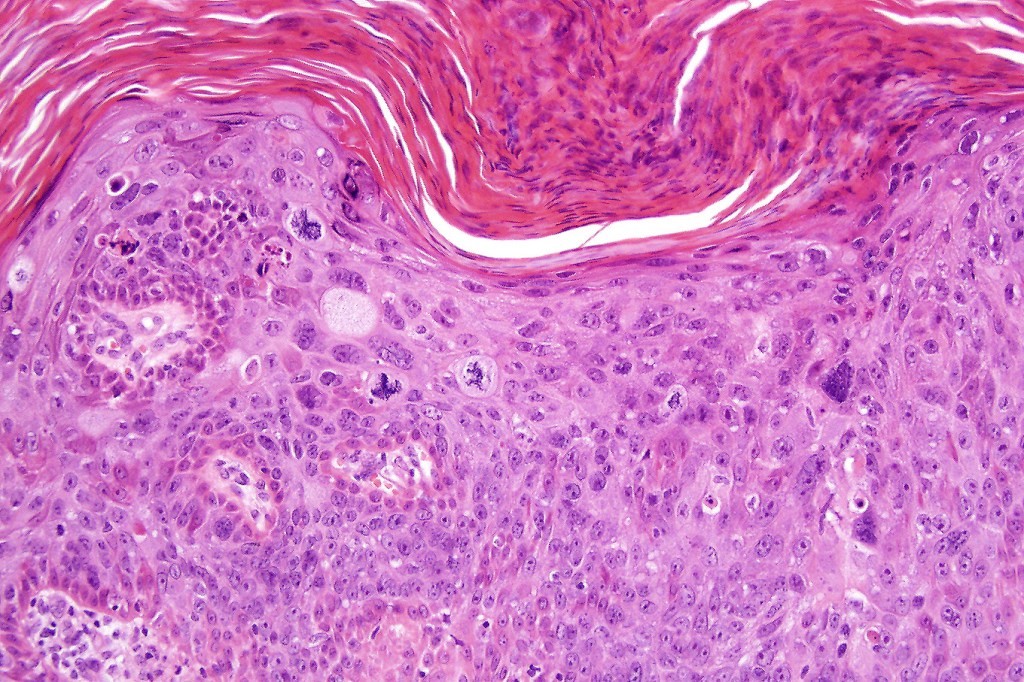
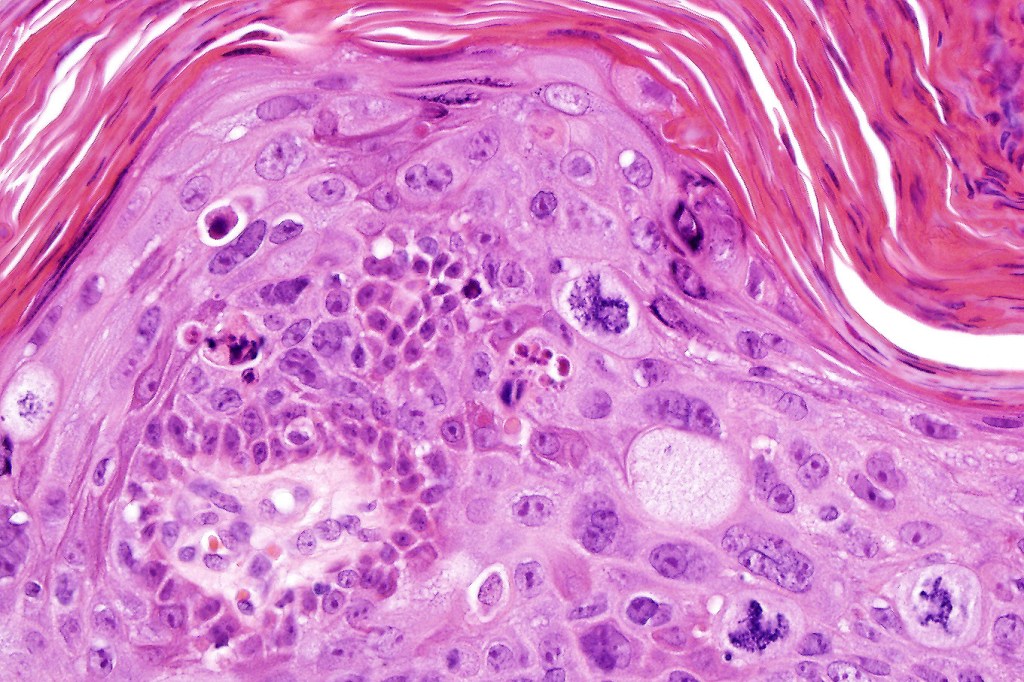
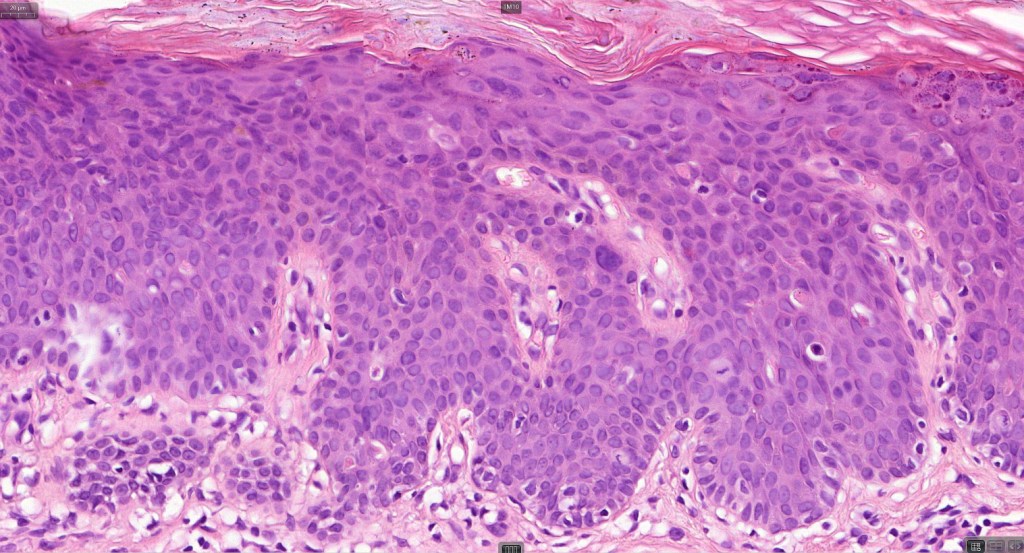
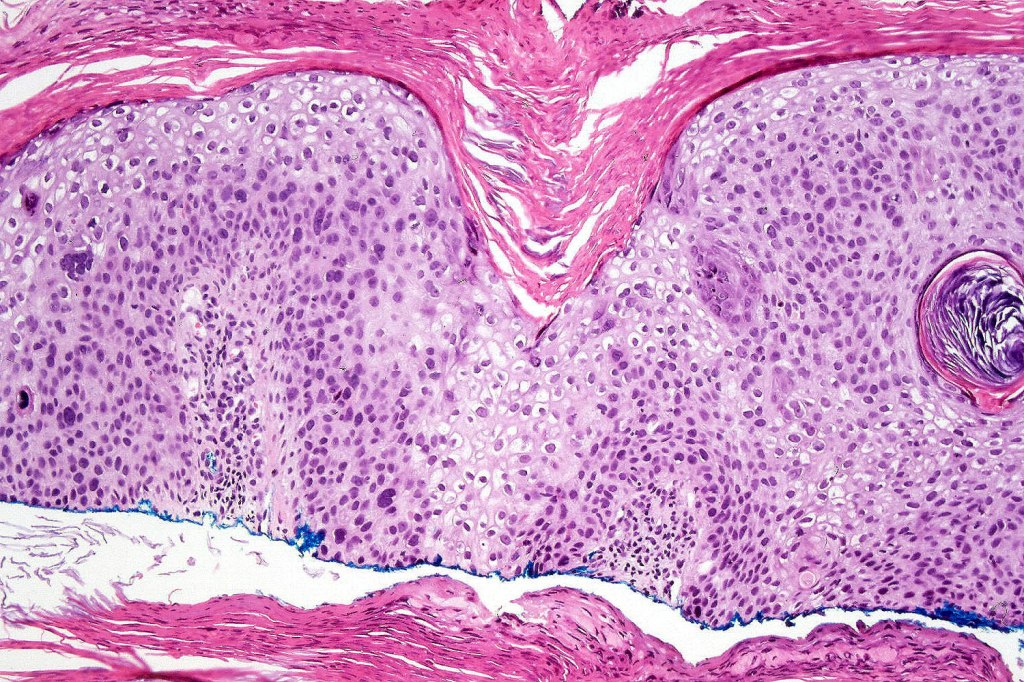
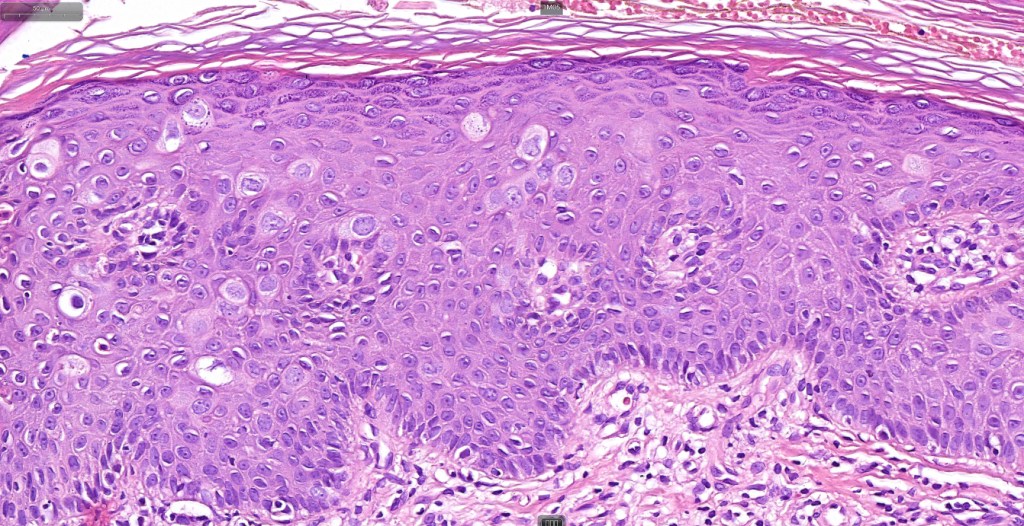
•Full thickness dysplasia (carcinoma in situ) involving the epidermis and intraepidermal adnexal elements
•Loss of maturation, nuclear pleomorphism, marked mitotic activity +/- abnormal forms
•Dyskeratosis & apoptosis
•Koilocytes in anogenital lesions
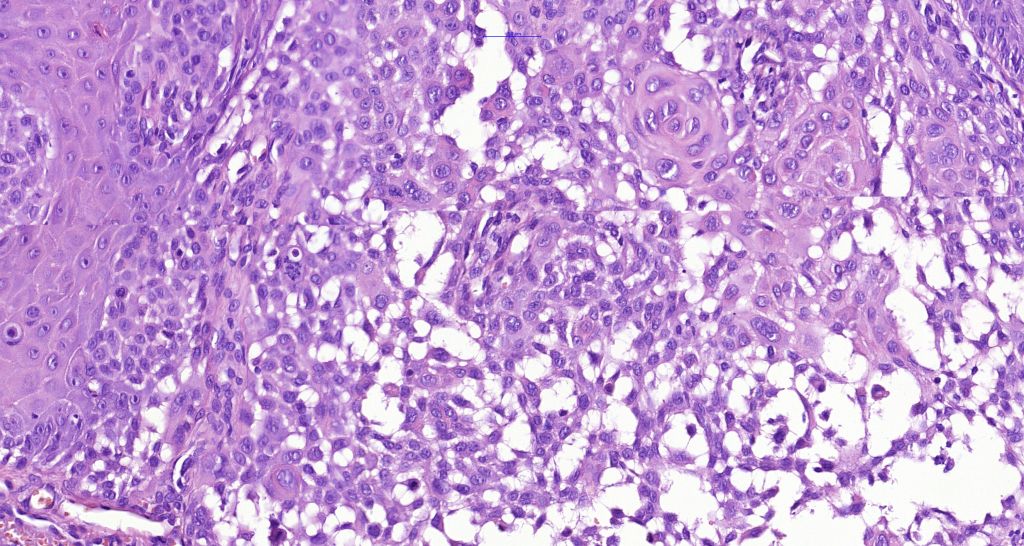
•Clear cell variant due to glycogen accumulation
•Acantholytic variant
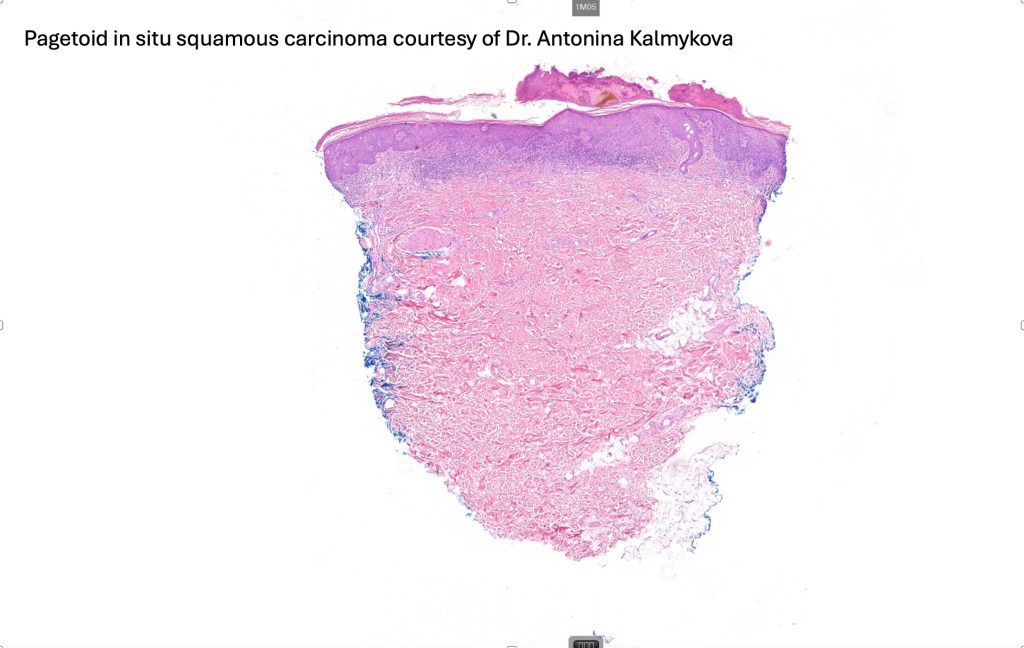
•Pagetoid variant
•Nested (clonal, Borst-Jadassohn) variant
•Lichenoid variant with interface change (lichenoid Bowenoid keratosis)
•Stromal amyloid deposition






















Differential diagnosis
Bowen’s disease is a clinical diagnosis and should not be used histologically. In situ squamous carcinoma is preferred. Since UV radiation is the most common cause of Bowen’s disease, it should come as no surprise that histologically it may be identical to Bowenoid actinic keratosis. If the dermatologist says it’s Bowen’s disease then that’s what it is. If the dermatologist says it’s an actinic keratsosis then that’s what it is!
Pigmented variants may be confused with melanoma and Pagetoid variants can be mistaken for extra-mammary Paget’s disease. Immunohistochemistry will solve any diagnostic dilemma.
Leave a comment